Surging coronavirus numbers threaten to exhaust local health care resources
If you have a loved one who has a heart attack today—or a stroke, or a wreck on iceslickened roads—you should worry about where they are going to go for the medical care they will need. It is a problem.
“We can get you to maybe Albuquerque or Kansas City or Tulsa or Little Rock,” said Hemphill County Hospital CEO Christy Francis, “but what’s going to happen while you’re trying to get them there…and then trying to get your insurance to pay the bill.”
Hospital administrators across the Texas Panhandle—whose acute care beds are full, whose medical and support staff are exhausted and, in some cases, sick or quarantined themselves, and whose resources are stretched to the breaking point—are all asking the same question.
This week, Francis sent an appeal for four additional nurses to the Emergency Operations Center for the Panhandle Regional Advisory Council. Her hospital staff is badly depleted. At least 15 staffers—over a third of them nurses—are unable to work, either because they have tested positive for the virus or have been quarantined due to close-contact with someone who has.
They are, for the most part, victims of the rapidly-accelerating community spread that has sent coronavirus case numbers soaring in Hemphill County, and in rural counties just like this one, all over the country [see story on next page].
Not only is the influx of virus cases affecting the ability to keep hospitals fully-staffed. It is also limiting their ability to treat patients who are in need of acute care.
“No patients are being accepted by the area hospitals that we usually transfer them to,” said Dr. Tony Cook. “If you don’t think that COVID is affecting you, think again.”
According to The Texas Tribune, hospitalizations and new cases are both at levels not seen since August. COVID-19 hospitalizations and the 7-day average of new cases have both risen more than 70 percent since the beginning of October. Experts blame sociallydense gatherings, like birthday parties and weddings, with the alarming increases in cases, along with widespread fatigue for following stringent public health guidelines.
Based on accelerating hospitalization, Dr. Cook said, and based on what we know, in three or four weeks, death rates will increase, as well. “We’ve learned a lot about treatment, like not using ventilators like we did,” said Cook. “But people are getting very sick and people are dying, and there just aren’t studies proving the efficacy of the drugs we are using.”
The rise of patients from rural areas with little health care infrastructure is overwhelming hospitals in larger cities. Officials in Amarillo’s hospitals are already sounding the alarm. “They are not going to be able to handle what’s coming our way,” said Francis. “They are talking about setting up alternative sites for patients.”
“We have contacted Dallas, Denver, Oklahoma City, Lubbock, and Midland-Odessa, trying to get some of our transfers out,” she said. “We have managed to get several out to Liberal, Kansas, and are very thankful.”
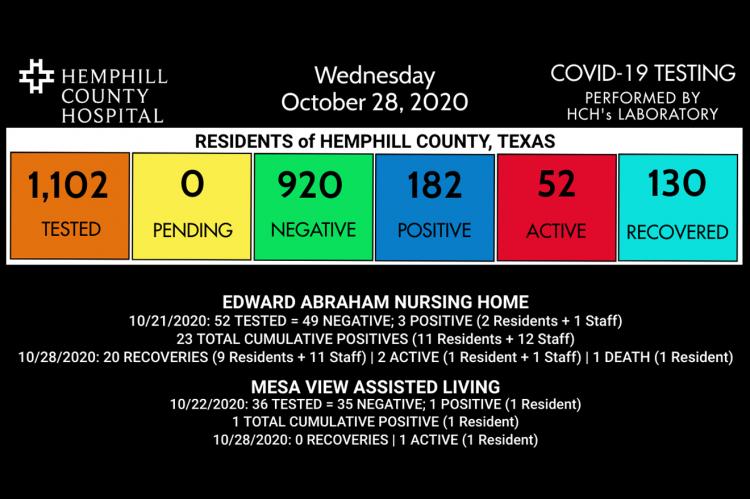
In the last seven days, the number of COVID-positive cases in Hemphill County has increased by 31. Hemphill County Hospital reported the first COVID-related death of an Edward Abraham Nursing Home resident this week, and its first coronavirus case in a resident of Mesa View Assisted Living. Canadian ISD has reported its 25th confirmed positive case. The number of out-of-county positive tests performed by the HCH lab continues to rise, as well, with 17 new ones in the last week.
County Judge George Briant and Mayor Terrill Bartlett teamed up this week, appealing to local residents to wear facemasks whenever possible. Though opposed to any government mandate, Briant urged the public to get back to practicing some of the things that were effective months ago, and proved to help. “We’re going to try to limit the velocity of it, and keep our health care facilities from being overwhelmed.”
“I do think wearing masks helps,” Bartlett said. “I don’t like wearing them. I don’t think anybody likes wearing them. It’s just something we need to do until we get a handle on this.”
“Logically, we’re going to see a delay in care,” said Francis, “not just for COVID, but for all illnesses.”
TO MASK OR NOT
If ever there was a hot-button topic, the wearing of face-coverings by the public is it. But despite heated political rhetoric and misinformation circulated on social media, evidence provided by infectious disease experts, including Dr. Francis Collins, Director of the National Institutes of Health, is clear: masking works. It’s among the easiest and most effective public health protocols available to combat the spread of COVID-19.
“The current surge in the Midwest is, unfortunately, entirely predictable,” Dr. Collins said Tuesday on NPR’s Morning Edition. “We never got on top of the virus to start with and we have not succeeded in introducing public health measures that really work, like masking, social distancing and hand-washing.”
“People are tired of the virus,” said Collins. “But the virus is not tired of us.”
Dr. Tony Cook, Hemphill County Hospital Chief of Staff is unequivocal in stressing the importance of donning a face-covering. “Masking is the most important thing we can do,” he said in a statement to The Record on Wednesday. “Handwashing, distancing, sure; but the more data we get shows the main thing is to wear a mask.”
As a trained healthcare professional, Canadian native Beverly Witcher Aycock, FNPC, sees lots of improperly-worn face coverings. “In nursing school, I was taught how to wear PPE (personal protective equipment) properly,” said Aycock. “Masks are only a barrier, they are not perfect and the wearer determines their effectiveness.”
“Surgical masks are disposable, to be used and tossed, protecting others from the wearer’s...germs but not perfect, because there is no seal,” she said. “To properly use a mask, it must cover the mouth and nose and it should not be touched once it is fitted.”
Touching the mask after putting it on, requires the wearer to wash their hands to prevent contaminating other surfaces. N95 masks protect the mask-wearer from others and must be worn tightly, sealed to the face. “They are not comfortable,” said Aycock. “Prior to COVID, they were primarily used with tuberculosis and chickenpox patients in isolation rooms.”
As a certified family nurse practitioner, Aycock concludes that all options are more protective than nothing, and masks—if worn properly—could make a difference in the spread of coronavirus. “Please stop readjusting or putting your hand inside them. They should be applied and left alone until removal,” she cautions. “Wash your hands and stay healthy.”
Becky Irvine RN, CHS Class of 1981, takes coronavirus seriously. “Our hospitals are maxed out. Medical staff exhausted, people are sick and dying yet people continue to negate hard work by saying this is no big deal, it’s not real, it’s all political,” she wrote. “Live in reality. Listen to science, your medical friends and neighbors. Please show you care about your sick and elderly who don’t have the luxury of pretending COVID is no big deal.”
“Stop whining about your perceived freedoms,” she concluded. “We can do what needs to be done to take care of each other.”